And Contribute to Hyperglycemia
Introduction to High Blood Sugar Levels [Hyperglycemia]
In the past, I have posted articles on impaired blood sugar levels that cause a condition called Diabetes. Today, in this article we are going to learn how the blood sugar levels are regulated by eight such organs and what causes these levels to rise [or fall] and the ways to manage it.
Hyperglycemia, commonly recognized as high blood sugar, is a condition that occurs when there is an excessive amount of glucose circulating in the bloodstream. This condition is often associated with diabetes, but it can also be influenced by various other factors and health conditions.
Maintaining balanced blood sugar levels is crucial for overall health, as glucose is a primary energy source for the body’s cells. Persistent hyperglycemia can lead to a myriad of health complications, including cardiovascular diseases, nerve damage, kidney failure, and vision problems.
The regulation of blood sugar levels is a complex process that involves multiple organs working in harmony. Disruption in the function of any of these organs can lead to hyperglycemia.
Which are the organs influencing blood sugar levels?
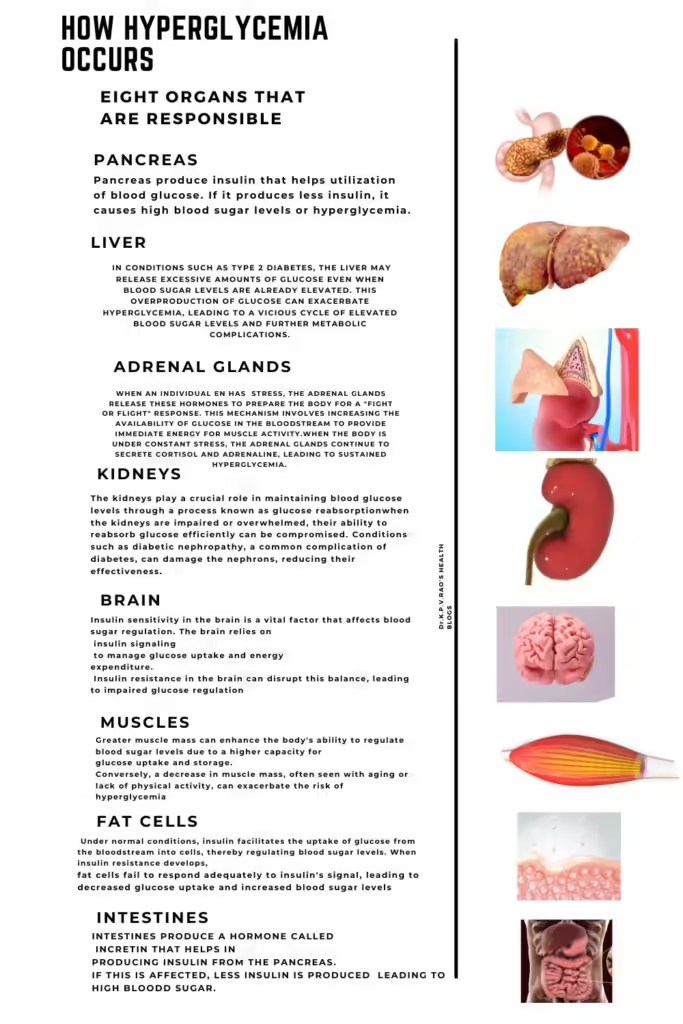
The pancreas, liver, muscles, adipose tissue, kidneys, brain, intestines, and skin all contribute to the delicate balance of glucose in the body. Each organ plays a unique role in either the production, storage, or utilization of glucose, and their coordinated efforts are essential to prevent hyperglycemia.
For instance, the pancreas produces insulin, a hormone that facilitates the uptake of glucose by cells. The liver stores glucose in the form of glycogen and releases it into the bloodstream as needed. Muscles and adipose tissues also store and utilize glucose, playing critical roles in maintaining blood sugar levels. The kidneys filter the blood, reabsorbing glucose and preventing its loss through urine. The brain, intestines, and skin are also involved in various metabolic processes that influence glucose levels.
Why is learning about these eight organs important?
Understanding how these eight organs influence blood sugar levels provides valuable insights into the multifaceted nature of hyperglycemia.
It highlights the importance of a holistic approach to health, where the functionality of each organ must be considered to prevent and manage high blood sugar.
In this blog post, we will learn the specific roles of these organs and how their dysfunction can contribute to hyperglycemia, offering a complete knowledge of the interconnected mechanisms regulating blood sugar levels.
As this article is quite exhaustive, let’s split it into two parts. In the first part we learn about the first four major organs, namely the pancreas, liver, brain, and the kidney’s role in regulating blood sugar levels and in the next part, we will learn how adrenal glands, fatty tissues, our muscles, and the intestines do it. So, let’s begin-
The Pancreas: Insulin Production and Release
The pancreas plays a critical role in maintaining blood sugar homeostasis through its production and release of insulin. This vital organ contains clusters of cells known as the islets of Langerhans, which house beta cells responsible for insulin secretion. Insulin is a hormone that facilitates the uptake of glucose by the body’s cells, allowing them to utilize glucose as a source of energy. When food is ingested, glucose levels in the bloodstream rise, prompting the pancreas to release insulin. This release signals cells in the liver, muscle, and fat tissue to absorb glucose, thereby reducing the concentration of glucose in the blood.
However, when the pancreas fails to produce adequate amounts of insulin or when the body’s cells become resistant to insulin, hyperglycemia can occur.
Hyperglycemia, defined as elevated blood glucose levels, can result from several pancreatic dysfunctions. One common issue is Type 1 diabetes, an autoimmune condition where our immune system mistakenly attacks and destroys insulin-producing beta cells. Consequently, in people with Type 1 diabetes, one must rely on external insulin administration to manage their blood sugar levels.
Another significant condition is Type 2 diabetes, where the pancreas produces insulin, but the body’s cells become resistant to its effects.
Initially, the pancreas compensates by producing more insulin, but over time, it may become overworked and fail to maintain the necessary insulin levels. This insulin resistance prevents cells from absorbing glucose efficiently, leading to persistent hyperglycemia.
Chronic hyperglycemia can have detrimental effects on various organs and systems, emphasizing the pancreas’s crucial role in regulating blood sugar levels.
Pancreas also produce glucagon in the alpha cells of the islet of Langerhans. This hormone acts on liver cells to release glucose stored as glycogen in liver cells [explained below].
To summarize, the pancreas’s ability to produce and release insulin is the basic requirement to prevent hyperglycemia. Changes in this process, whether due to autoimmune destruction, insulin resistance, or any other factors, can significantly impact blood sugar regulation and contribute to the development of diabetes and related complications.
Useful Article: How Insulin and Glucagon regulate Blood Sigar
The Liver: Glucose Storage and Release
The liver plays a pivotal role in maintaining blood sugar levels through two primary processes:
- Glycogen storage and
- Glucose release.
Glycogen, a polymer of glucose, is stored in the liver and acts as a reserve of energy that can be mobilized when the body requires additional glucose. This storage mechanism is crucial for ensuring a steady supply of glucose, particularly between meals and during physical exertion.
So, how does the liver regulate blood sugar levels?
When blood sugar levels drop, the liver responds by breaking down glycogen into glucose through a process known as glycogenolysis. This glucose is then released into the bloodstream to provide a quick source of energy. Glycogenolysis is a rapid response mechanism, ensuring that the body can maintain homeostasis and meet its energy demands promptly. The hormone glucagon from the pancreas helps in this process.
In addition to glycogenolysis, the liver can also produce glucose from non-carbohydrate sources through a process called gluconeogenesis. This involves converting amino acids, lactate, and glycerol into glucose, which can then be released into the bloodstream.
Gluconeogenesis is particularly important during prolonged fasting or intense physical activity, where glycogen reserves might be depleted.
However, the liver’s ability to release glucose can become a contributing factor to hyperglycemia when it is dysregulated. In conditions such as type 2 diabetes, the liver may release excessive amounts of glucose even when blood sugar levels are already elevated. This overproduction of glucose can worsen hyperglycemia, leading to a vicious cycle of elevated blood sugar levels and further metabolic complications.
Therefore, understanding the liver’s dual role in glucose storage and release is essential for managing blood sugar levels effectively. By regulating these processes, it is possible to mitigate the risk of hyperglycemia and maintain overall metabolic health.
The Kidneys: Glucose Reabsorption
The kidneys play an important role in maintaining blood glucose levels through a process known as glucose reabsorption. This intricate procedure begins in the nephrons, the functional units of the kidneys. As blood flows through the glomeruli, the initial filtering units, glucose is filtered out of the bloodstream along with other substances.
However, under normal physiological conditions, the majority of this glucose is reabsorbed back into the bloodstream through specialized transporters in the renal tubules. This reabsorption process ensures that glucose is not lost in the urine and is available for the body’s energy needs.
How do the kidneys regulate blood sugar levels?
The primary mechanism of glucose reabsorption involves sodium-glucose cotransporters (SGLT) located in the proximal convoluted tubule of the nephron. These transporters facilitate the movement of glucose from the filtrate back into the blood. Specifically, SGLT2 reabsorbs around 90% of the glucose, while SGLT1 accounts for the remaining 10%. This highly efficient system is crucial for maintaining normal blood glucose levels.
However, when the kidneys are impaired or overwhelmed, their ability to reabsorb glucose efficiently can be compromised. Conditions such as diabetic nephropathy, a common complication of diabetes, can damage the nephrons, reducing their effectiveness.
When the blood glucose levels exceed the renal threshold, typically around 180 mg/dL, the transporters become saturated, and glucose begins to spill into the urine, a condition known as glucosuria. This excess glucose in the urine is a hallmark of hyperglycemia and can lead to further complications if not managed properly.
Moreover, certain medications that inhibit SGLT2, known as SGLT2 inhibitors, are used therapeutically to manage hyperglycemia by promoting the excretion of glucose in the urine. While effective, these medications highlight the delicate balance the kidneys must maintain in glucose reabsorption to avoid contributing to hyperglycemia.
The Brain: Appetite Regulation and Insulin Sensitivity
The brain plays a crucial role in the regulation of appetite and insulin sensitivity, significantly influencing blood sugar levels. The hypothalamus, a critical region of the brain, is responsible for processing signals related to hunger and satiety.
When the body senses a drop in blood glucose levels, the hypothalamus triggers the release of hormones that promote feelings of hunger, prompting food intake. Conversely, when blood glucose levels rise, the hypothalamus releases hormones that signal satiety, helping to control food consumption.
Insulin sensitivity in the brain is a vital factor that affects blood sugar regulation. The brain relies on insulin signaling to manage glucose uptake and energy expenditure. Insulin resistance in the brain can disrupt this balance, leading to impaired glucose regulation.
When the brain becomes less responsive to insulin, it can result in increased appetite and overeating, further contributing to hyperglycemia. This insulin resistance can also impair the brain’s ability to regulate peripheral glucose metabolism, promoting high blood sugar levels.
Additionally, the brain’s communication with other organs through the autonomic nervous system is essential for maintaining glucose homeostasis.
Dysregulation in these neural pathways can lead to improper signaling between the brain and the pancreas, liver, and muscles, further contributing to hyperglycemia.
These neural dysfunctions can disrupt the delicate balance required for optimal blood sugar control, making the management of hyperglycemia more challenging.
To summarize, understanding the brain’s role in appetite regulation and insulin sensitivity is crucial for developing effective strategies to combat hyperglycemia. By addressing neural mechanisms and improving insulin sensitivity in the brain, it may be possible to enhance overall glucose regulation and reduce the risk of long-term complications associated with high blood sugar levels. This highlights the importance of considering the brain’s influence when developing comprehensive approaches to managing hyperglycemia.
To be concluded….
In my next article we will discuss the remaining four organs that regulate blood sugar levels. You can opt to get notification by subscribing to the notification by clicking on the bell icon in the article.
Adios.