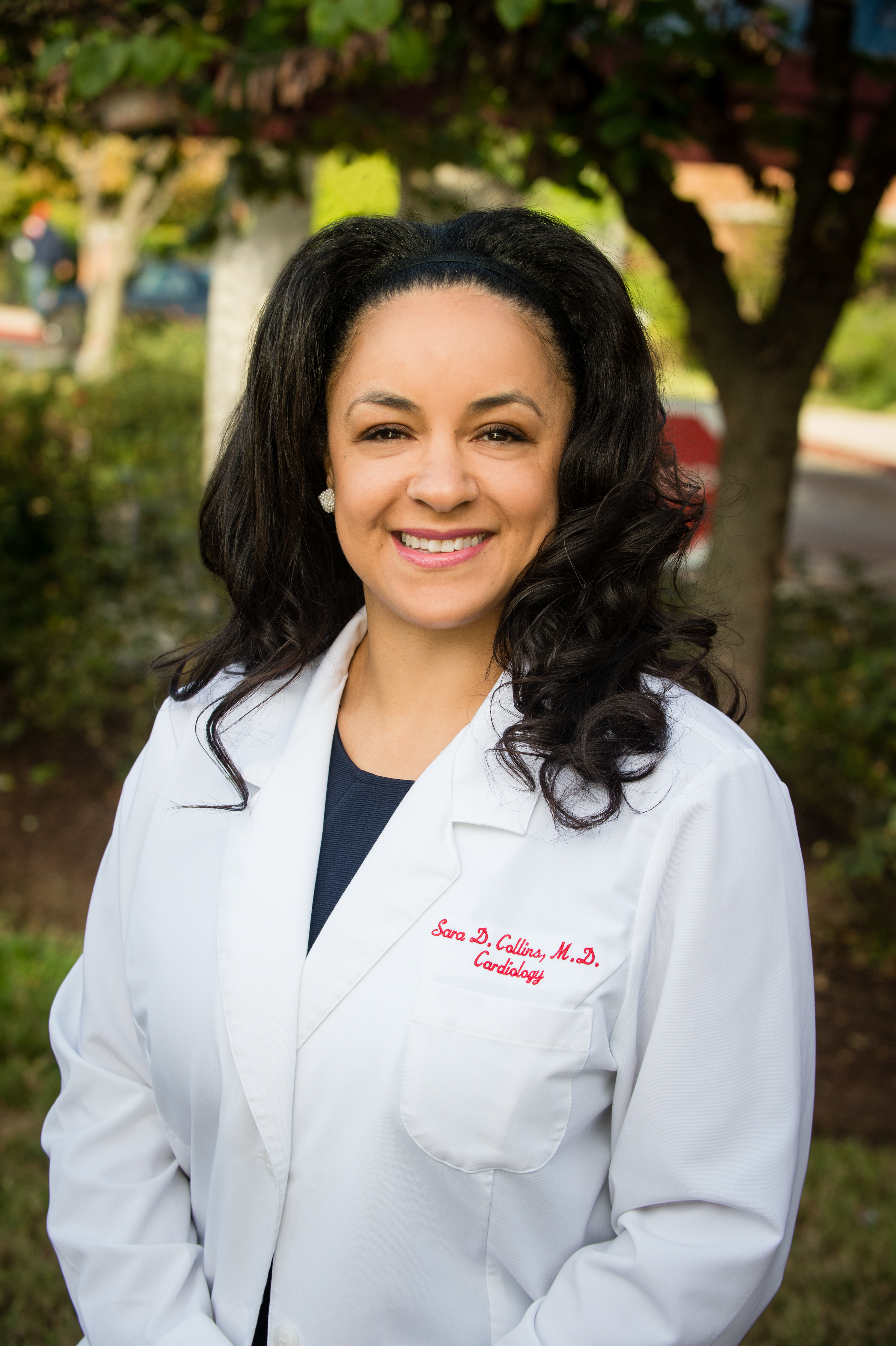
Dr. Sara Collins is an Interventional Cardiologist in Bowie, Maryland. She earned her undergraduate degree from Brown University and her medical degree from Meharry Medical College. She completed her Internal Medicine training at the University of Maryland Medical Center, Cardiology fellowship at Georgetown University/Medstar Washington Hospital Center, and Interventional Cardiology training at Medstar Washington Hospital Center.
Dr. Collins has been involved in research for over 25 years. Her research has included vaccine development, observational studies, clinical device investigations, and phase II through IV clinical pharmaceutical research. She founded the Capital Research Institute, which was created to conduct cardiovascular clinical trials in Washington, D.C.
Dr. Collins serves as a consultant for healthcare startups engaging in business and product development. She is an active member of the association of Black Cardiologists and co-chairs their Health and Public Policy Committee.
Elevated Lipoprotein(a), often referred to as Lp(a), has been recognized as a significant risk factor for heart disease. Dr. Sara Collins, interventional cardiologist and researcher, breaks down the importance of knowing your Lp(a) levels, understanding your risk, and keeping hope alive.
Dr. Collins is working towards fostering a research community that is racially diverse and hopes to chip away at health disparities by addressing minority underrepresentation in clinical trials.
“There are many different types of cholesterol in our bodies. Some are worse than others. Lp(a) is one type of bad cholesterol,” said Collins. “Lp(a) levels are determined genetically, meaning they are inherited. The amount of lipoprotein(a) you have as a child will most likely be the level you have life long.” She emphasizes that Lp(a) levels can vary depending on race or ethnicity, and people of African descent tend to have the highest levels of Lp(a).
Lp(a) is measured with a simple blood test, but it is not a test that is usually done routinely. You may have to ask your healthcare provider if this test is appropriate for you based on your risk, and request to have this specific test done if so. At this time, the test does not need to be repeated like other cholesterol tests; however, that may change once treatment options are available. Knowing your Lp(a) level is a major part of understanding your risk.
Dr. Collins explains that Lp(a) differs from other types of cholesterol in that levels are not affected by changes in diet and exercise habits. Your Lp(a) may be high even if you live a healthy lifestyle. “Most of the patients that I diagnose with elevated Lp(a) also have some risk factors they can modify,” she stated, “Even if Lp(a) levels are elevated, you should still practice healthy lifestyle habits like healthy eating and exercising regularly.”
Doing so will still help decrease your overall risk and improve your heart health. “You don’t want to make things worse by eating a diet that’s high in saturated fat and not exercising,” said Collins. She highlights that the biggest risks associated with elevated Lp(a) are blood clots, inflammation, and plaque buildup.
Until therapies are approved to treat elevated Lp(a) levels, we must understand our risk both personally and as a community so that we can take action. Taking action may include evaluating your health history to determine if you are at risk, taking steps to introduce healthy lifestyle habits, or getting your levels checked. Clinical trial participation is another practical step you can take if you have been diagnosed with elevated Lp(a) or are at risk for certain heart conditions such as heart disease, stroke, or peripheral artery disease.
“African Americans are overrepresented when it comes to the burden of heart disease, but none of the treatments that we use have been appropriately studied in us,” said Dr. Collins. “The mistrust when it comes to healthcare and clinical research is valid and it’s real, and we have to chip away at it.” How do we do that? One way is by participating in clinical trials.
Did you know that by participating in clinical trials, you can help researchers develop new treatment options? Minorities are often underrepresented in clinical research, despite having higher rates of conditions being studied. This makes participation a crucial but collective community effort that can help improve our overall health in the long-term and promote better health outcomes.
Dr. Collins encourages and advocates for minority clinical trial participation. She states, “When you enroll in a clinical trial, you’re in a very supported, safe, observed, and regulated clinical environment. Additionally, you’re not only doing a service to yourself, but you’re also doing a service to your community.”
Clinical research studies are investigating cardiovascular disease and risk factors associated with it, including Lp(a). Learn more at Lilly Clinical trials.
